Bloating is a frustrating symptom of eating disorders. It can show up with an active eating disorder or at any point during recovery. It is uncomfortable, embarrassing, and can make recovery even harder (hello bad body image!)
This article will outline what bloating is, the causes of it, potential treatments, and how to cope with bloating during eating disorder recovery.
Table of Contents
What is bloating?
“Bloating” is a vague term that my clients use to describe anything from gas, swelling, water retention, and abdominal distention (i.e. sensation that your stomach is sticking out).
Bloating is extremely common among those recovering from an eating disorder.
Causes of bloating during eating disorder recovery
There are several causes of bloating during eating disorder recovery. However, I want to point out that bloating is actually a symptom of the eating disorder itself. Many of these symptoms resolve as recovery progresses.
Delayed gastric emptying
Delayed gastric (or stomach) emptying, also known as gastroparesis, is a side effect of food restriction. The body compensates for a reduced food intake by slowing down digestion. As a result, food sits in your stomach and gastrointestinal tract longer. This can make it seem like your stomach is protruding for an extended amount of time following a meal.
Delayed gastric emptying also leads to increased gas production. Under normal conditions, the bacteria in your gut will ferment the food fibers in your colon which produces gas. When foods sit in your colon for longer, there is a greater opportunity for fermentation to occur.
Muscle breakdown from malnutrition
Malnutrition can cause muscle breakdown throughout the whole body. This can happen to the muscles in your digestive tract as well. As a result, food is not moved through digestion as quickly or efficiently. This can lead to increased bloating and gas.
High fiber intake
Many of my clients with disordered eating eat a diet very high in fiber. While fiber is important to healthy bowels (among other things!), high fiber consumption in the absence of adequate food and calories can lead to increased gas, bloating, cramping, and constipation.
Medication side effects
Certain medications used to treat underlying anxiety and/or depression such as tricyclic antidepressants can contribute to constipation and associated bloating/gas.
That being said, PLEASE consult your medical provider before changing your medication regimen!
Electrolyte imbalances
Restriction and vomiting (intentional or spontaneous) can lead to depletion of the electrolytes potassium and magnesium. This depletion can interfere with nerve functioning in your colon and slow things down.
Laxative abuse
Laxatives are used to stimulate a bowel movement. A history of laxative overuse/abuse can damage the nerves in your gut. This can lead to long-term constipation and a dependency on laxatives.
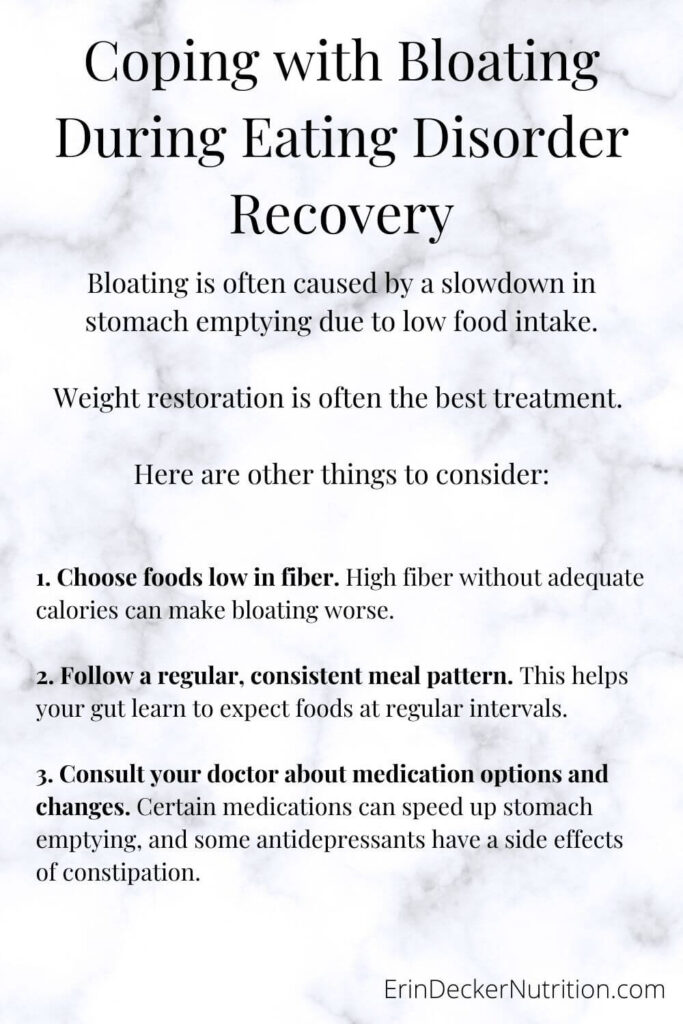
Treatment for bloating during eating disorder recovery
The treatment for bloating during eating disorder recovery will depend on what the cause of the bloating is.
For many, achieving a biologically appropriate weight will resolve nearly all gastrointestinal problems. This will reverse malnutrition, allow for muscle growth and recovery, normalize electrolytes, and allow the gut to adapt to a consistent, reliable meal pattern.
Unfortunately, weight restoration takes time and dealing with bloating can slow this down. Luckily, there are a few things that can make the process a bit smoother.
How to minimize bloating during eating disorder recovery
- Choose foods lower in fiber. Say what?? I know – fiber is supposed to maintain healthy bowel movements. However, in this case, fiber may just make your bloating worse. Choose more refined grains and fewer fruits and vegetables.
- Follow a regular, consistent meal pattern. This helps your gut learn to adapt to and expect foods at regular intervals.
- Talk to your doctor about changing up your medications. For example:
- Use of an osmotic laxative instead of a stimulant laxative. Osmotic laxatives are those that pull water into the gut rather than stimulate the nerves to move your bowels. Examples of osmotic laxatives include miralax and milk of magnesia.
- Ask about metoclopramide, a medication that can speed up stomach emptying time.
- If you are taking a tricyclic antidepressant, ask if there are alternatives that do not contribute to constipation.
Should you do an elimination diet during eating disorder recovery?
Elimination diets such as the low FODMAP diet are common suggestions to minimize bloating, gas, and other digestive complaints. However, in the case of eating disorder treatment, I cannot recommend this approach.
As I’ve described above, specific foods are not the cause of bloating during eating disorder recovery. It is a normal response to restriction and malnutrition. Ironically, doing an elimination diet may just make your symptoms worse.
Final Note
Bloating is a completely normal, albeit uncomfortable part of eating disorder recovery. Talk to your treatment team about medication options and alternatives if needed. Most importantly, know that in many cases, the bloating is temporary and just a part of the process. In the wise words of Virgil: “the only way out is through!”
Looking for a dietitian to join your treatment team? Reach out today!

So if I don’t worry about it, my bloated tummy will go away over time?
Hi Tulasi,
This is hard to say since I don’t know you personally. It really depends on your stage of recovery. Most people find it goes away as they continue to progress in recovery (for all the reasons I outlined). But I also know that for some, the bloating may have been a contributing factor to their ED in the first place. So in that case, recovery won’t necessarily fix the issue, but it will definitely help! I recommend speaking with your treatment team if you have one, or reaching out to a dietitian skilled in this if it’s accessible for you.
Good luck ❤️
Hi! I’ve had particularly bad bulimia throughout 2023, binging/puging was so extreme I quickly lost weight and had symptoms like dizziness, numb extremeties, amenorrhea, etc. I’ve been in on-and-off recovery for the past couple of months, and have been completely b/p free for about three weeks. And I’m so gassy! My gas doesnt stay in the gut, I’m farting and burping constantly 😂 Will this eventually go away? I gained a bit of weight back as I started recovery and most of the other symptoms are gone. I just hope the gas also dies down so I wont embarass myself someday.. ED starts with low self-esteem anyways and the gas does not help!
Hi Jess,
First of all, CONGRATS on B/P free for 3 weeks! (maybe longer at this time of writing?)
And OH man I’m so sorry you’re struggling with this! You’re right – gas gas and burping are embarrassing, albeit normal body functions. If you were having physical symptoms from your ED, it is very possible you had some muscle wasting as well. Weaker muscles in you gut and pelvic floor can definitely contribute, and will take more than a few weeks to recover.
I didn’t spend much time on this in the post and in hindsight I wish I had – sometimes these symptoms are a factor in the ED development in the first place. If these symptoms existed before your ED, it’s possible that they won’t fully resolve just with normalization of eating (though keep in mind recovery will help!! restriction will guaranteed make it worse).
Definitely share your concerns with your treatment team if it feels safe for you. It can certainly be a barrier to recovery.
Good luck!!
Hi! I’ve had particularly bad bulimia throughout 2023, binging/puging was so extreme I quickly lost weight and had symptoms like dizziness, numb extremeties, amenorrhea, etc. I’ve been in on-and-off recovery for the past couple of months, and have been completely b/p free for about three weeks. And I’m so gassy! My gas doesnt stay in the gut, I’m farting and burping constantly 😂 Will this eventually go away? I gained a bit of weight back as I started recovery and most of the other symptoms are gone. I just hope the gas also dies down so I wont embarass myself someday.. ED starts with low self-esteem anyways and the gas does not help!
My daughter, who is 13, has had an ongoing eating disorder (AN) for 18 months now. We are currently in the ‘refeeding phase’ and she has healthily gained 6kg. The problem now for her is, she is negatively drawn to her ‘bloated’ stomach. This bodily change has inadvertently played havoc on her mental state. She hates feeling bloated, often refuses to shower and will only brush her teeth with the lights off so she can’t see herself in the mirror. Her eating disorder is telling her she’s so bloated and big. Please send some advice the ways how to inform daughter why she’s experiencing this. Thank you